Published:
The Covid-19 pandemic created an explosion in the use of disposable face masks around the globe.
This added to the already significant amount of PPE waste generated by hospitals and in other medical settings.
Researchers from Heriot-Watt University have developed a process that degrades a common face mask using the power of fresh air and 200W of electricity - about the same as a small microwave.
Our low-power air plasma method efficiently degrades surgical masks in four hours, so that 90% of the mask is gone.
The team's findings are reported in the academic journal Materials Degradation.
Dr Humphrey Yiu, assistant professor at Heriot-Watt University, said: “PPE from the healthcare sector has always been a waste challenge. It's high-volume and must be treated as biohazardous waste, which means it is incinerated.
“Incineration is expensive and not environmentally friendly - reaching the high temperatures required, over a long period of time, uses a lot of energy and generates a significant amount of pollutants.
“We proved that our small-scale, cold plasma system can degrade single-use face masks, the use of which has exploded since the pandemic. They are still widely used around the world.
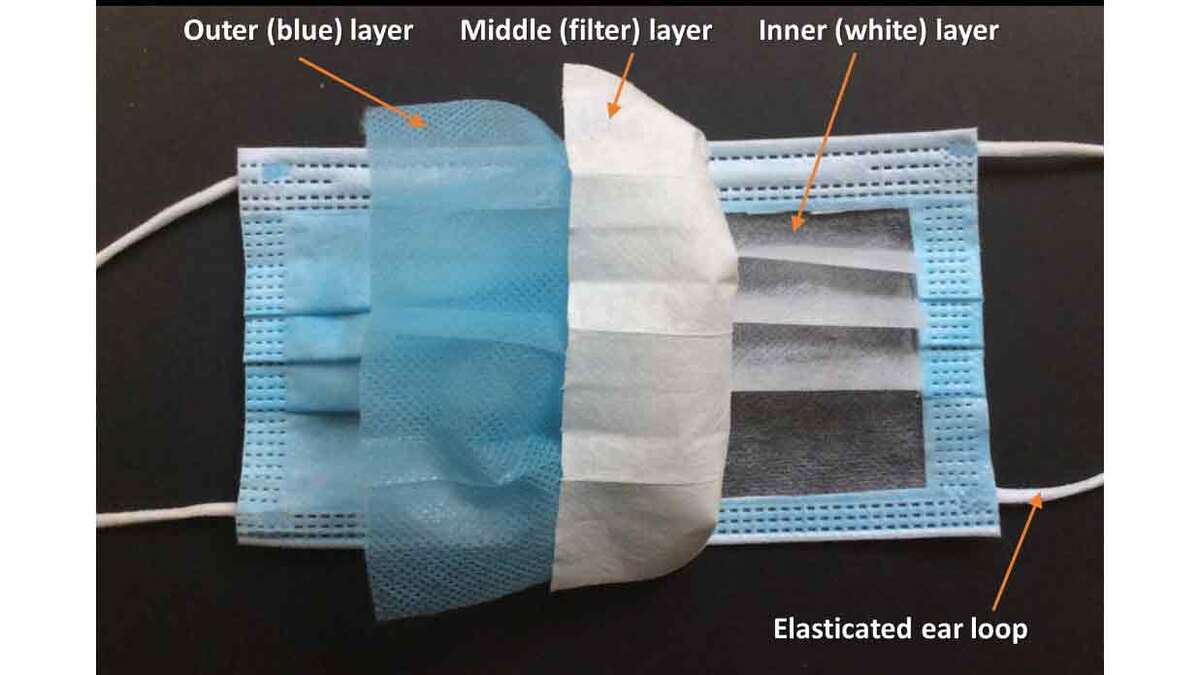
“Our low-power air plasma method efficiently degrades surgical masks in four hours, so that 90% of the mask is gone.”
The Heriot-Watt air plasma system is mains-powered and produces a highly reactive environment rich in oxygen atoms that etches the plastics in the mask and eventually converts them into carbon dioxide and water.
Professor Martin McCoustra, who specialises in complex surfaces research, said: “Plasma is already used to decontaminate surfaces as it destroys biological materials like bacteria and viruses as easily as any plastic.
“In this work, we've gone beyond simple decontamination to actually break down waste material by exposing the waste to the plasma for longer and at higher applied powers.
The small-scale system has limitations, the researchers point out.
Dr Humphrey Yiu said: “The ear loops on the masks were extremely stubborn, we could only degrade those by 9%.
“Our focus now is scaling up the system to prove that the system could work at the hospital scale. We'd like to develop models that could be installed in hospital wards or GP practice rooms, or work at the hospital scale, where hundreds of tons of PPE need to be destroyed.”
Dr Yiu and the team are applying for funding for the next stage of the research.