Unheard voices reshape health and care in pioneering arts research project
Clubs, schools, day centres and other community settings could help to make health and care more accessible, new research suggests.
Familiar places like these could remove barriers to care, like not being sure if there is a health or care issue, where to go, how to get there, who to see or what to tell the health or care practitioner.
This is one of more than 20 recommendations made by people across the UK who researchers say are rarely consulted about the design of health and social care services.
The people in our study are from communities which aren’t often listened to or included in discussions about the design of health and care services.
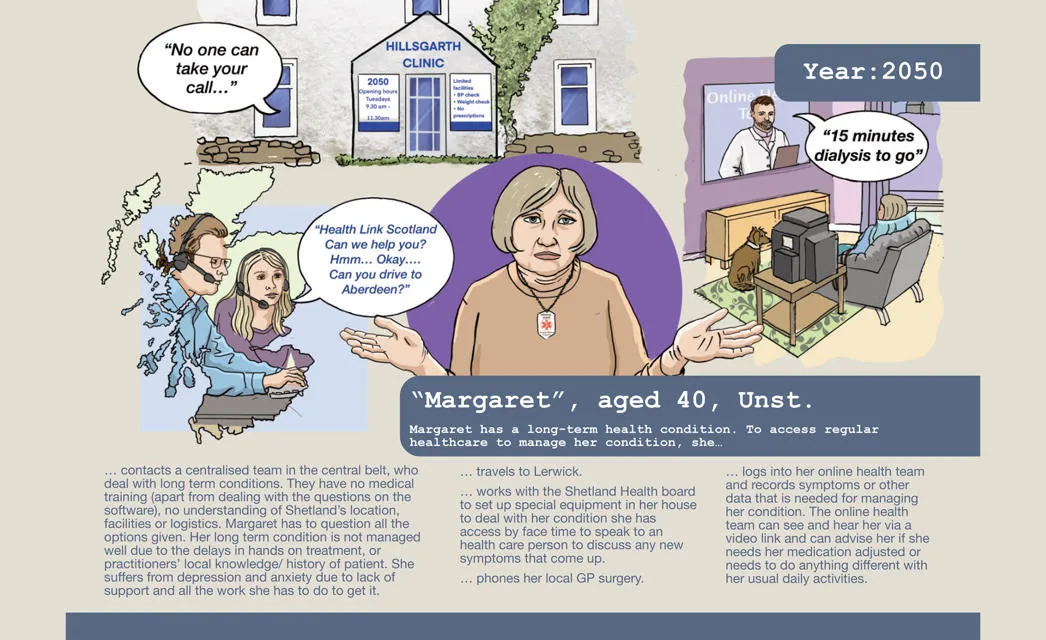
A new report coins the term ‘seldom-listened-to’ to describe these people and communities. The researchers also coin the term ‘health labour’ to describe the effort needed by seldom-listened-to people to access health and care.
The report, titled Designing the future of care with seldom-listened-to people, encompassed ten projects across the UK, from Kent in south east England to the Highlands and Islands in Scotland.
Participants in the research included siblings of children with life-limiting conditions; women, trans men, non-binary, and gender nonconforming people with energy limiting chronic illness, such as Long Covid and autoimmune conditions; older autistic people with learning disabilities; people living with chronic inflammatory disease, endometriosis; rural communities in the Highlands and Islands of Scotland; diverse communities in Greater Manchester; children living in areas of high deprivation in the South Tees region; African-Caribbean communities in London; mental health service users in Kent and both patients and staff who are staying or working in care units in hospitals.

“The people in our study are from communities which aren’t often listened to or included in discussions about the design of health and care services,” explained Professor Mary Stewart, academic lead for the project and Director of Social Interaction, Mental Health and Wellbeing at Heriot-Watt University in Edinburgh. “And yet these communities can experience profound health and care inequalities that can impact on their physical and mental health, quality of life, and the ability to live well – not only for the individual – but also their families and the wider community.
“Our research sets out the specific ways in which staff, organisations, stakeholders, and policymakers can place seldom-listened-to individuals and communities at the heart of the design of the future of health and care.
“We show not only that this is possible – but that it’s vital to co-design the future of health and care with these people and communities to improve health and care for everyone.”

The report is part of research funded by the UKRI Arts and Humanities Research Council (AHRC) – which supports arts and humanities research and study in the UK – and uses creative methods to explore how seldom-listened-to people and groups would like the future of health and social care to look.
Instead of using traditional research methods like surveys and interviews – which aren’t always accessible to seldom-listened-to people – the researchers worked with artists and creative methods to capture the views and experiences of participants. These creative methods included film, music, poetry, podcasts, comics, creative writing and folk stories.
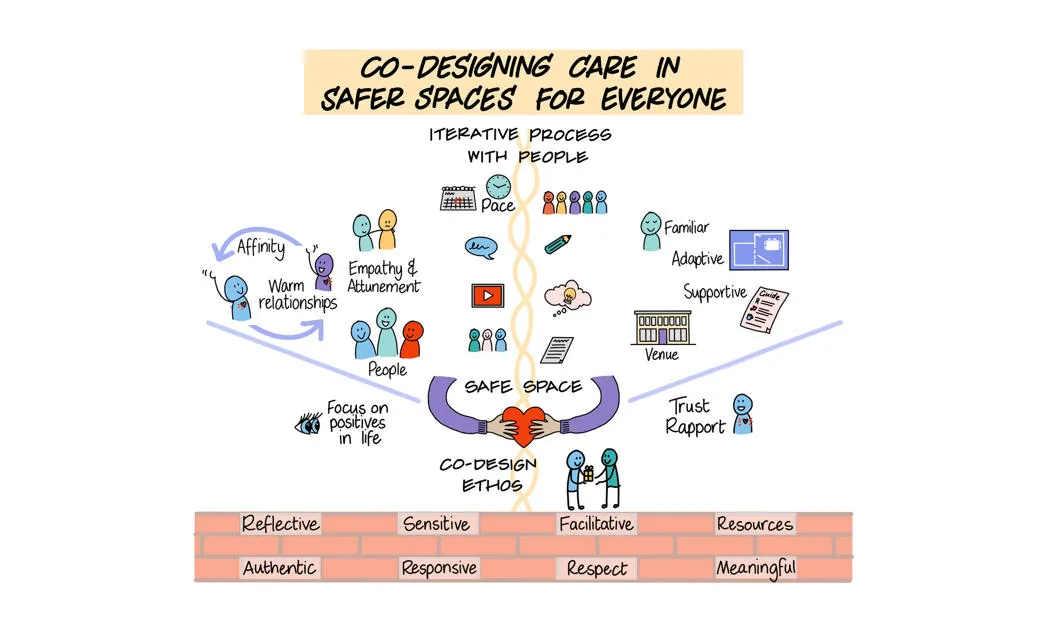
Through a series of activities and workshops, the seldom-listened-to participants ‘reimagined’ health and social care services which could give them more say in decision-making, help them to access and engage with care – and use safer spaces to build trust and rapport.
Research co-author Bryony Nisbet, a Psychology Research Assistant at Heriot-Watt University, explained: “By safer spaces, we mean community places that are already familiar to people, and where they may already have support from trusted others. For example, if you’re an autistic adult with learning disabilities, accessing health and care in a day centre you already attend potentially removes the huge physical and sensory overload of trying to get to and navigate around a new place you’ve never been to before. For the NHS and social care, the practical change we’re proposing is moving the point of care from GP surgeries into the community. This in turn can help to tackle the growing burden on primary care in the UK.”
Other recommendations in the report include providing multidisciplinary services that span sectors including housing, employment and education – alongside health and care.
Care should also anticipate future needs, for example by developing ‘future-ready homes’ that are already adapted to meet the needs of vulnerable groups as they get older.
The report also recommends that professionals are trained to work with people with varying communication, cognitive, sensory and cultural needs.
The research aligns with the UK government’s 10-year plan to bring the NHS closer to home, including neighbourhood health centres which will house services under one roof and will be open at evenings and weekends. The researchers have written a policy brief detailing their recommendations for policymakers. This will be shared with politicians across the UK, including Members of the Scottish Parliament and Members of Parliament at Westminster.
The ten projects in the research were all partnerships between communities, community organisations and universities. The other university partners were University of Liverpool, University of Greenwich, Strathclyde University, Edge Hill University in Lancashire, University of Manchester, Manchester Metropolitan University, Teesside University, University of Kent and UHI Inverness, part of the University of the Highlands and Islands.
The organisations and charities involved in the research included disability group Chronic Illness Inclusion; Manchester public arts project We Live Here; charity Endometriosis UK; Scottish Autism; educational institution Tees Valley Education Trust; singing for wellbeing workshop specialist, Everyone's A Singer; Caribbean community group, Caribbean Social Forum; arts community outreach project, Inverness Openarts and many others.
Participants in the research included Oliver Waite, who took part in University of Manchester’s research project, called NHS 75/150 Looking Back, Looking Forwards. This engaged diverse communities in Greater Manchester in discussions around the future of health and care. Oliver’s story is captured in a comic-book style artwork that highlights the importance of seeing people as individuals.
Oliver explained: “I have schizoaffective disorder, I’m autistic and I’ve transitioned from female to male. But I’m more than just a list of medical issues. I’m a part-time history student with the Open University, I build models, such as Lego, and I play wheelchair rugby league.”
Dr Myrtle Emmanuel, Associate Professor in Human Resource Management & Organisational Behaviour at the University of Greenwich, led a research project called Re-igniting Windrush folk stories and songs to improve African-Caribbean mental health disparities in the London Boroughs of Lewisham and Greenwich.
She said: “African-Caribbean communities are 40% more likely than white British people to come into contact with mental health services and to be detained under the Mental Health Act. Our project looked at a different approach, one that builds on the cultural traditions and community support that have always helped people stay mentally well. Through storytelling and folk song workshops, we created a practical toolkit to help promote good mental health in local communities”
Dr Rachel Carroll, an Associate Professor in English at Teeside University, led a research project called, Empowering children to shape the future of research on social inequality, health and wellbeing. She said: “The children and young people in our project were able to explore and express their lived experiences and perspectives on social inequality and health and wellbeing through a series of interactive and inclusive workshops, including comic-making, creative writing, dance and performance. We hope the artworks, creative writing and films that captured their voices will help health professionals, policy makers, researchers and the wider public to learn from the experience and insights of children and young people.”
In their report, the researchers say their term ‘Health Labour’ represents “the burden on the individual and those associated with the individual to access and navigate care.”