PhD researcher harnesses AI to transform skin cancer diagnosis in remote areas
A researcher at Heriot-Watt University is harnessing the power of artificial intelligence to give patients living in remote parts access to timely and potentially lifesaving medical diagnosis.
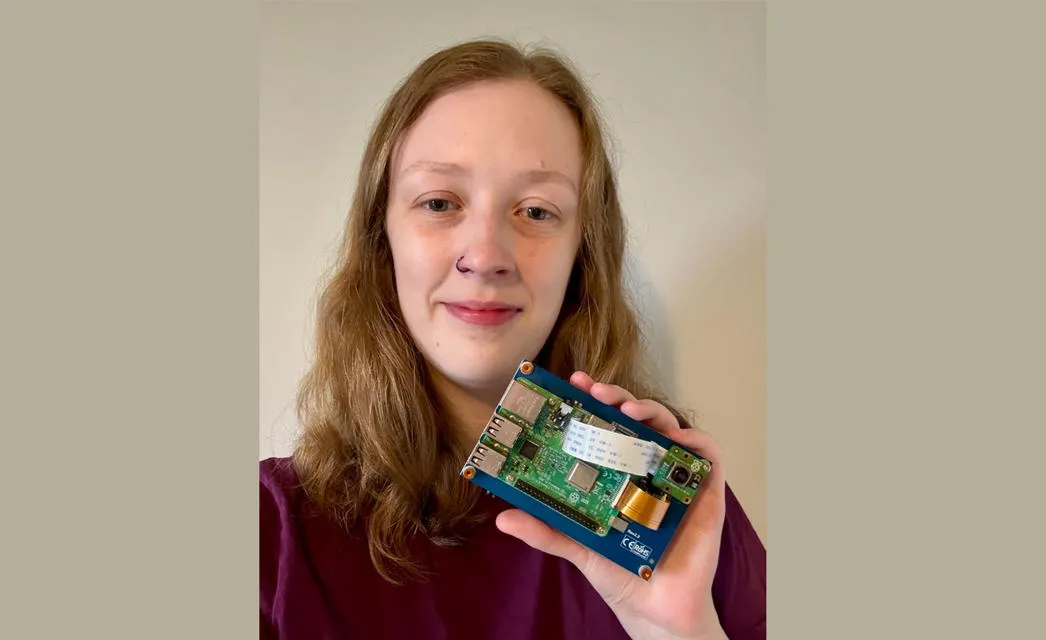
For the past two years, Tess Watt, a PhD candidate in the School of Mathematical and Computer Sciences based in Edinburgh, has developed AI-driven tools to diagnose skin conditions, most notably skin cancer, in areas with limited medical infrastructure.
If we can empower people to monitor skin conditions from their own homes using AI, we can dramatically reduce delays in diagnosis.
Her goal is to enable early detection without the need for direct access to dermatologists, using accessible technology that could be deployed anywhere from rural Scotland to West Africa.
"Healthcare from home is a really important topic at the moment, especially as GP wait times continue to grow," said Tess.
"If we can empower people to monitor skin conditions from their own homes using AI, we can dramatically reduce delays in diagnosis."
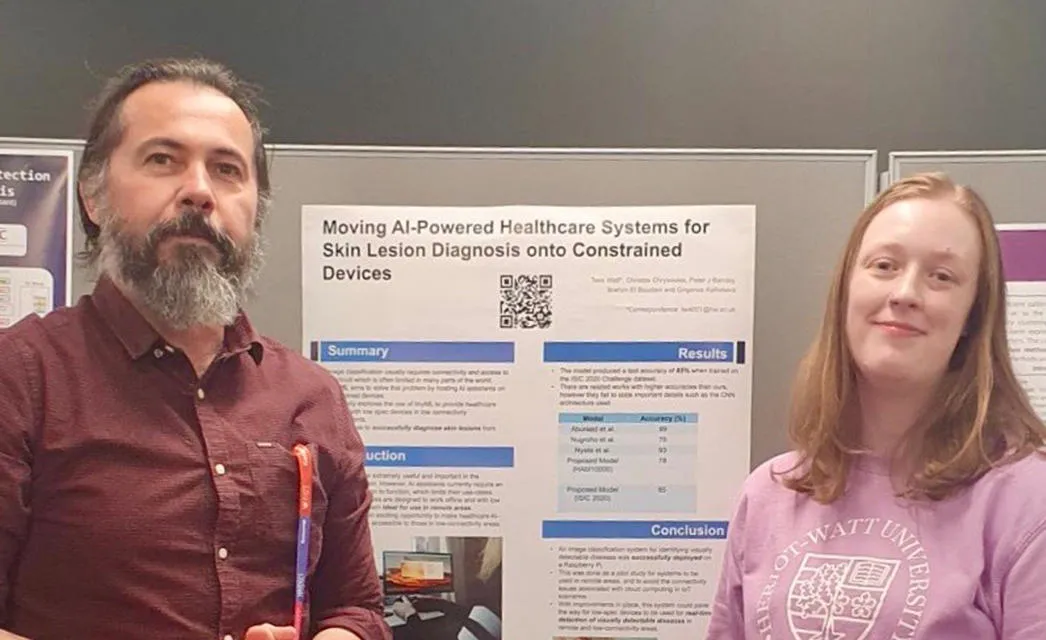
Tess is leading the pioneering research in a broader collaborative effort involving academics at the London South Bank University, Edinburgh Napier University and the Foundation for Research and Technology – Hellas in Greece. The project has received funding through the Engineering and Physical Sciences Research Council (EPSRC) the main funding body for engineering and physical sciences research in the UK and part of UK Research and Innovation (UKRI), the UK’s national funding agency for investing in science and research.
It is understood to be the first research project of its kind to combine AI medical diagnosis with the aim of serving remote communities.
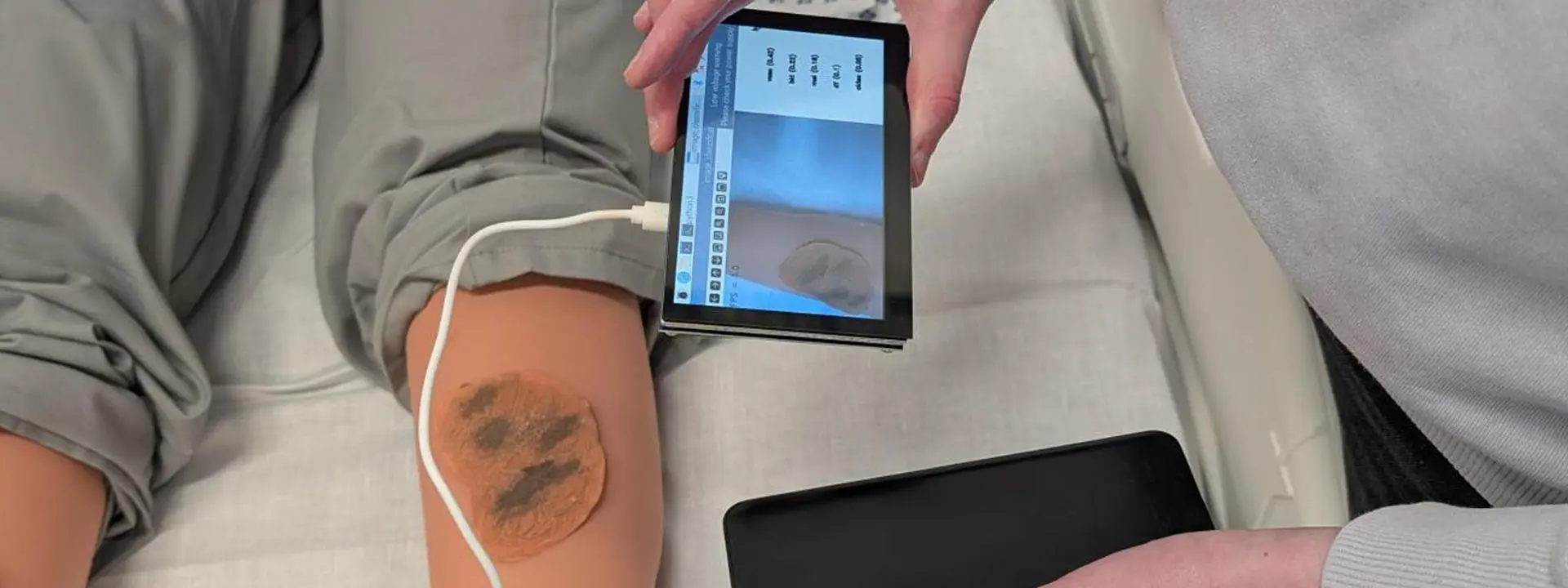
A prototype of her system has already been demonstrated at Heriot-Watt’s advanced health and care technologies suite, showcasing how AI can analyse images of skin lesions and flag potential risks for further medical review.
What sets the system apart is its ability to work without the need for internet access.
Using low-cost Raspberry Pi devices, the technology can diagnose a skin condition whilst working independently of WiFi. A Raspberry Pi can be thought of as a handheld portable computer that is energy efficient and capable of storing a vast amount of information in its memory.
A patient equipped with one of these devices would be asked to take a picture of their skin complaint using a small camera attached to the Raspberry Pi. This is analysed in real-time using the latest state-of-the-art image classification, comparing it to an enormous dataset of thousands of images to reach a diagnosis.
The findings are then shared with a local GP service to begin a suitable treatment plan.
The tool is up to 85% accurate in its diagnostic capabilities but the team intends to increase this percentage further by gaining access to more skin lesion datasets aided by advanced machine learning models.
While the technology has yet to be tested in real-world clinical settings, Tess is currently in talks with NHS Scotland to begin the ethical approval process.
"Hopefully in the next year or two, we'll have a pilot project underway," she said, noting that medical technology often takes years to move from prototype to implementation.
The long-term vision is to roll the system out first across remote regions of Scotland, before expanding to global areas with limited access to dermatological care. It could also offer vital support to patients who are infirm or unable to travel, allowing loved ones to assist with capturing and submitting diagnostic images to GPs.
Tess’s journey into healthcare AI was inspired by earlier work in accessible translation technologies.
That experience, coupled with her current studies in Tiny Machine Learning and research into underexplored areas of AI in medicine, led her to focus on dermatology.
"There's a lot being done with AI and medical scans like X-rays and MRIs," she said, "but relatively little using photographs of skin.
“I saw a real opportunity there."
Though deployment may be years away, the relevance of her work is immediate. As health services across the UK struggle with backlogs and stretched resources, solutions that enable proactive, remote care are increasingly in demand. Tess’s research could represent a major step forward in both equity and efficiency for healthcare delivery.
As the technology matures and collaboration with the NHS progresses, Tess remains committed to ensuring that her research has a tangible impact by the time she graduates. "By the time I finish my PhD, three years from now" she said, "I’d love to see something well into the pipeline that’s on its way to real-world use."
Commenting further on the project, Tess’s academic supervisor, Dr Christos Chrysoulas, Associate Professor of Computer Science at Heriot-Watt University’s School of Mathematical and Computer Sciences, emphasised the importance of robust system design in healthcare technology.
“E-health devices must be engineered to operate independently of external connectivity to ensure continuity of patient service and safety,” he said.
“In the event of a network or cloud service failure, such devices must fail safely and maintain all essential clinical operations without functional degradation.
“While auxiliary or non-critical features may become temporarily unavailable, the core diagnostic and even therapeutic capabilities must remain fully operational, in compliance of course with safety and regulatory requirements.
“Ensuring this level of resilience in affordable, low-cost medical devices is the essence of our research, particularly for deployment in resource-limited settings and areas with limited or no connectivity, where uninterrupted patient care must still be guaranteed."

Tess’s work forms part of Heriot-Watt’s wider ambitions to make a positive impact on lives through its Global Research Institute (GRI) in Health and Care Technologies, which is dedicated to advancing solutions for some of the world’s most critical health challenges.
The Institute is helping deliver pioneering research across Heriot-Watt’s campuses in Scotland, Dubai and Malaysia, whilst working closely with health and care industry partners around the world. It is already making significant progress with the launch of "One Health", an established research theme within the GRI that is addressing global health challenges such as infectious diseases, antimicrobial resistance (AMR), and emerging epidemics through the integration of human, animal, and environmental health.